When the COVID-19 pandemic hit last year, people had to stop gathering indoors. That meant big changes for the All of Us Research Program. In March 2020, we had to pause our in-person recruitment and enrollment efforts.
In February, All of Us partners were meeting with people daily, inviting them to learn more and to join the program. We were enrolling up to 900 people like you every day. To enroll, many participants went to partner sites to give blood and urine samples. They also stopped by to get help with online surveys. The surveys covered their health, medical history, and other topics. Then much of the United States began to hunker down and socially distance. We paused all in-person activities so we could protect public health.
We didn’t know how long the pandemic would last. But we started thinking about how to reopen when it became safe to do so.
We created a team to come up with a safe process to reopen the brick-and-mortar sites. The team started planning in April 2020. With so many unknowns about the virus, the team focused on safety. That meant safety for participants, safety for staff, and safety for surrounding communities.
The plan was to reopen in phases, starting in July 2020. Sites with fewer COVID-19 cases in their surrounding communities could reopen first. The sites used sources such as Covid Act Now’s color-coded tracker to decide where it was safest.
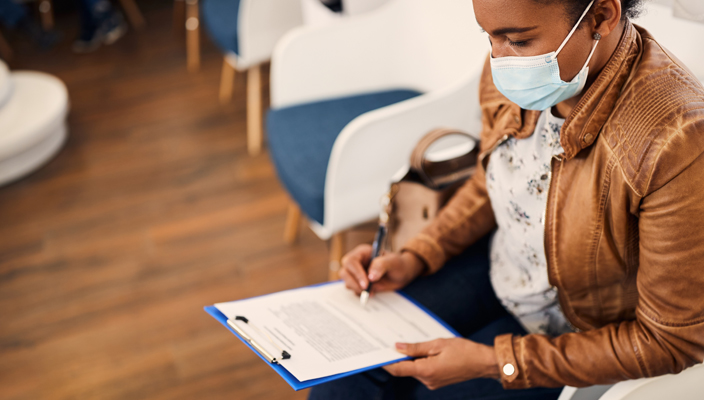
The team used safety guidelines from the Centers for Disease Control and Prevention (CDC). Staff would have to wear hospital-grade masks. Participants also would have to wear masks. The sites needed to have enough room for social distancing. Some sites asked that participants wait in their cars until staff was ready for them.
Closing down sites for at least four months affected some people more than others. Most of our activities were online. Participants who didn’t have access to computers or didn’t use them all the time were doing fewer activities.
At the same time that sites were starting to reopen, the team began testing a few pilot programs to make staying involved easier. One pilot program let some people donate saliva at home rather than coming in to give a blood sample.
For online tasks, All of Us started a program called CATI to help reach those without access to the internet or who don’t use computers much. CATI stands for Computer Assisted Telephone Interviewing.
In CATI interviews, a participant gets a phone call from a staff member. The staff member has been specially trained on the surveys and in computer security. The staff member reads the survey questions to the participant. As the participant answers, the staff member enters the responses and can clarify questions.
So far, the CATI pilot has gotten wonderful feedback from participants. Comments include, “This was easier than getting my brother to help me,” and, “This was helpful. I don’t have a computer.”
The pandemic pilot programs are winding down as reopening continues. As of July 6, 2021, 179 sites in 19 states have reopened, and another 94 have plans ready to go. The sites use checklists to make sure they have all requirements covered.
Once the pandemic recedes, All of Us will have decisions to make. How many of the new services should we keep (and maybe expand) for the rest of the program? These services include things like CATI.
“Given that we’ve made many changes during the pandemic, things won’t go back exactly to the way they were,” says Sarra Hedden, Ph.D., one of the reopening team project leads. “For some sites, we’ll have more ways they can take part in the program. Ones that don’t require in-person activities. The pandemic has gotten us thinking of ways to make it easier for participants to be involved.”
It’s not just the enrollment sites that are opening their doors again. Community sites have been planning ways to safely reopen in person. Some All of Us partners took part in the Healthy Families Expo in Waco, Texas, in early June. The expo shared health information, provided services like blood pressure screenings, and held giveaways. The Temple Missionary Baptist Church in Duncanville, Texas, rallied the public with Let’s Get Moving Through the Pandemic. There, attendees could sign up to receive the COVID-19 vaccine. All of Us also joined Our Community Health Festival in New Orleans, Louisiana. At the festival, guests could learn more about All of Us and sign up for the program. And in Corona, New York, the National Alliance for Hispanic Health hosted the 15th Annual ¡Vive tu vida! Get Up! Get Moving!®. Attendees had access to no-cost health screenings, health information, All of Us information, and COVID-19 vaccines.
We know we’re not out of the pandemic woods yet. We know some areas are still struggling to get vaccinations up and COVID-19 cases down. But we can’t hide our excitement at seeing All of Us participants like you face to face again.
If you’re unable to enroll in person, you can still sign up and participate online at JoinAllofUs.org.